Researchers are active in finding new drugs, and new purposes for existing ones. As drugs are being developed, and existing drugs explored for use with other conditions, clinical trials are conducted to test their safety and effectiveness.
Clinical trials are the final step in a long process that begins with research in a lab. Before any new treatment is used with people in clinical trials, however, researchers work sometimes for many years to understand its effects on cancer cells in the lab and in animals. They also try to figure out the side effects it may cause. This is called the preclinical phase.
When a drug is ready to be tried on people, the drug’s developer will initiate a clinical trial. Trials are available for all stages of cancer, not just those who have advanced cancer that is not responding to treatment.
Clinical trial are usually conducted in phases. Regardless of the phase, safety is the most important, and the trial will stop if there are serious side effects.
Phase 1
Phase I of a trial is done to find the highest dose that can be given safely without causing severe side effects. The doses are stepped up. The first participants get a very low dose, then it is increased for each new group. The phase continues until researchers find a dose that might likely work without severe side effects.
Because there are a small number of participants in a phrase I trial, rare side effects might not show up until later phases.
Some phase I trials include participants with different cancers. The primary concern is safety.
Even though the goal of this phase is treatment, but tolerance, some patients join them. If the other recommended treatments have failed, there may be a benefit to join a phase. Of course, there may be a trial in a later phase that may be more desirable.
Phase 2
If a new treatment is found to be safe in phase I clinical trials, a phase II clinical trial is done to see if it works in certain types of cancer. This might mean it shrinks the cancer, or it puts it in remission so it doesn’t grow or return for a period of time. Every participant usually gets the same dose of the drug.
Because a greater number of participants are in this phase, less common side effects might be seen. If participants benefit from the drug, without serious side effects, a phase III trial will be conducted.
Phase 3
Treatments that have been shown to work in phase II clinical trials must succeed in one more phase before they’re approved for general use. Phase III clinical trials compare the safety and effectiveness of the new treatment against the current standard treatment.
Because doctors do not yet know which treatment is better, study participants are often picked at random to get either the standard treatment or the new treatment. When possible, neither the doctor nor the patient knows which of the treatments the patient is getting. This type of study is called a double-blind study.
Most phase III trials are conducted at multiple locations to get the most number of participants, sometimes at local hospitals or doctors offices. Some studies pick patients at random to receive a placebo, a harmless drug to see if there is any psychological effect. At some point in time, however, they may be allowed to receive either the standard or the new therapy
FDA Approval and Phase 4
When a phase 3 clinical trial shows a new drug is more effective or safer than the current treatment, the developers apply for FDA approval to make it publicly available. If approved, the drug can then be used for the disease the drug was tested on.
If the FDA feels that more evidence is needed to show that the new treatment’s benefits outweigh its risks, it may ask for more information or even require that more studies be done, even after it approves the drug for use. This continued surveillance effort would be considered Phase 4 of the clinical trial.
Joining a Clinical Trial
You can search for clinical trials by going to https://clinicaltrials.gov
Every trial has a person in charge, usually a doctor, who is called the principal investigator. The principal investigator prepares a plan for the trial, called a protocol. The protocol explains what will be done during the trial. It also contains information that helps the doctor decide if this treatment is right for you. The protocol includes information about:
- The reason for doing the trial
- Who can join the trial (called eligibility criteria)
- How many people are needed for the trial
- Who to contact to join.
- Any drugs or other treatments that will be given, how they will be given, the dose, and how often
- What medical tests will be done and how often
- What types of information will be collected about the people taking part.
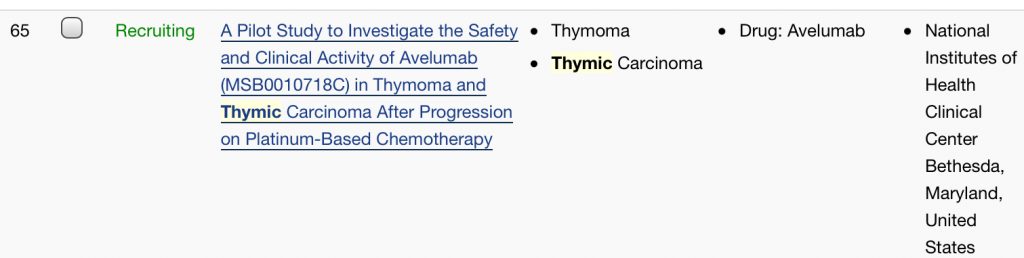
For each trial, the listing will show its status. This includes:
- Completed
- Recruiting
- Unknown
- Terminated)
- Active, not recruiting
- Enrolling by invitation
- Not yet recruiting
- Withdrawn
Select a study to see detailed information including eligibility criteria and contact information.
Compassionate Drug Use
During the clinical trial, a drug is called investigational and only available to the trial participants. Compassionate drug use means making a new, unapproved drug available to treat a seriously ill patient when no other treatments are available.
Drugs that are being tested but have not yet been approved by the US Food and Drug Administration (FDA) are called investigational drugs. These drugs are normally available only to people who are taking part in a clinical trial.
Patients with serious or life-threatening conditions who can’t get treatment with an unapproved drug through a clinical trial might benefit from compassionate use. This involves getting special permission from the FDA.
There are two ways to apply for the drug, both initiated by your doctor’s office.
- Through expanded access programs (EAPs).
- Through Right to Try.
Expanded access programs (EAPs)
This program is run buy the FDA, which approves most of these requests when patients meet all of these conditions.
- Have a serious and life-threatening condition
- Are not eligible for any current clinical trial that’s using the drug
- Have no other comparable treatment options
- Are likely to have benefits that outweigh the risks involved
The Right to Try Act
Under a federal law passed in 2018, patients can go directly to the drug company without going through the FDA. The Right to Try Act doesn’t give you the actual right to try any drug, it just lets you apply to the drug company without FDA guidance.
It’s important to understand that Right to Try does not actually give patients the right to try any unapproved drug they wish to try. Instead, it gives them the right to request access to an unapproved drug from the company that makes it, without having to go through the FDA.
You can be turned down by the drug company for a variety of reasons. You must meet the requirements spelled out by the law, and the drug company can just refuse or be unable to make enough to honor all requests.
To be eligible for Right to Try, a patient must:
- Be diagnosed with a life-threatening disease or condition
- Have tried all approved treatment options for the disease or condition
- Have a doctor certify that they are unable to participate in a clinical trial for the investigational drug
- Give written informed consent that they understand the risks of taking the investigational drug
- The drug must have gone through at least a successful phase 1 trial.