Some patients with thymoma or thymic carcinoma, about 30%, have no symptoms when it is diagnosed. These are typically detected when doctors are looking for other things, such as a routine chest x-ray.
With other patients, typical symptoms include:
- Persistent Coughing
- Chest pain
- Upper airway congestion.
- Muscle weakness
- Fatigue
- Shortness of breath
- Arm or facial swelling
- Difficulty swallowing
- Anemia (low red blood cell count)
- Increased risk of infection
Because these same symptoms could point to many conditions, thymoma is often not considered until other causes have been exhausted. Ironically, symptoms like these also point to autoimmune diseases, such as myasthenia gravis. Since those are often linked with thymoma, doctors will look for thymoma as a cause.
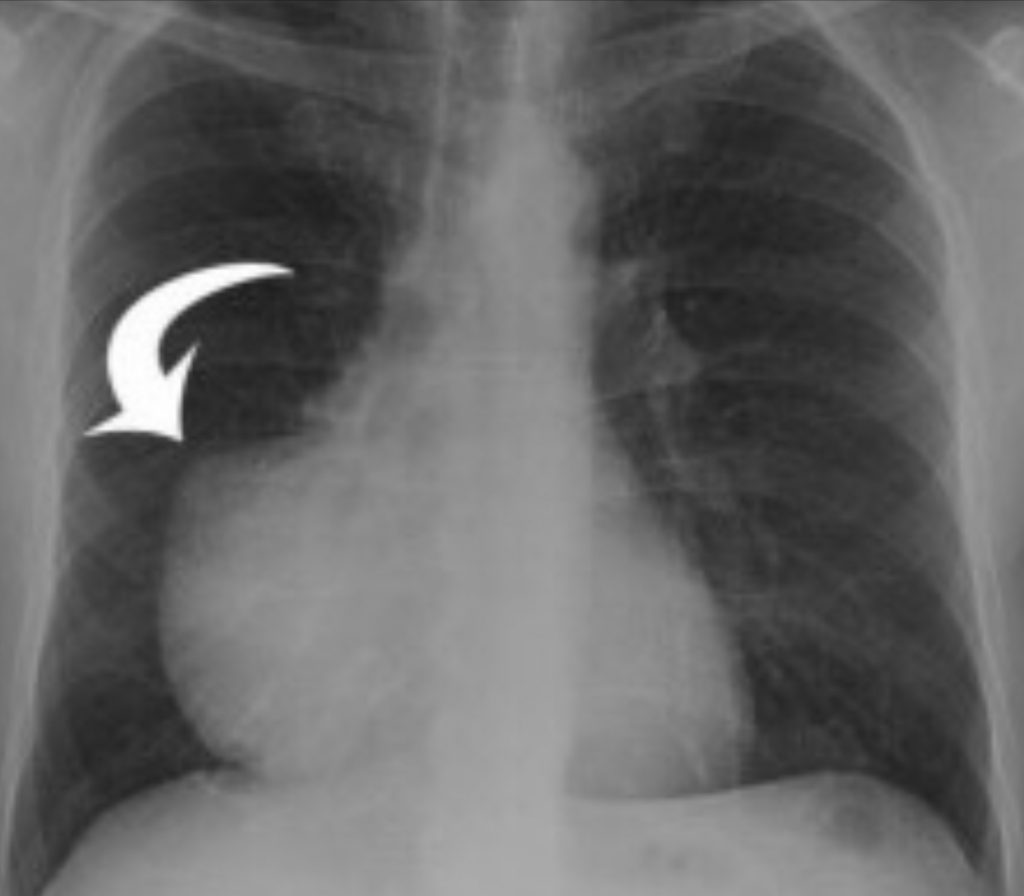
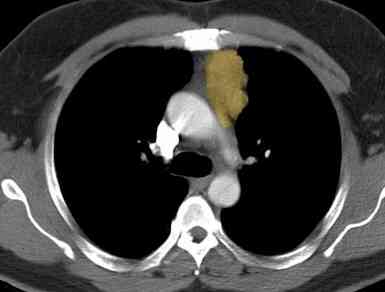
Your doctor will use a variety of methods to diagnose your condition. These include blood tests, X-rays, CT scans, MRIs, and PET/CT scans to determine the size and position of the tumor.
The PET scan can help determine if there are potentially any cancer cells in the tumor or elsewhere. When you have the PET scan, a small amount of a radioactive solution is injected into a vein. Because cancer cells take in the solution when normal cells won’t, they appear on the scan. Today, one single scan does a combination of both a CT and PET.
If a thymic tumor is likely, they will determine if it is operable and the best method to use for the surgery. If the tumor seems inoperable because of its size and location, then radiology and/or chemotherapy may be considered.
If it is unlikely that the tumor is thymic, or it is not operable, the doctor may order a biopsy. Ultrasound-guided fine needed aspiration biopsies can go directly to the tumor with the least invasivemess. The samples will be sent to a pathologist who determines what type of tumor it is.
The Question of Biopsies
Whenever a biopsy is performed, there is always a fear that it will dislodge cancer cells so they spread to other parts of the body. This is called seeding. Because of this possibility, the NCCN guidelines are very clear when it comes to biopsies.
 The guidelines say that biopsies should be avoided if the tumor is strongly suspected to be a thymoma and it is resectable. The rationale behind this is that the tumor needs to be surgically removed anyway, so why go through an additional procedure.
The guidelines say that biopsies should be avoided if the tumor is strongly suspected to be a thymoma and it is resectable. The rationale behind this is that the tumor needs to be surgically removed anyway, so why go through an additional procedure.
If a biopsy is performed, then the guidelines stress to avoid a transpleural (through the pleural surrounding the lung) because of the “substantial risk of converting a stage I thymoma to a stage IV thymoma by spreading tumor within the pleural space.”
Differential Diagnosis
Many times a particular set of symptoms can point to a number of different causes. For efficiency, the most likely causes are considered first. The doctor will orders tests, scans, or whatever they need to confirm, or to reject, their suspected diagnosis. Sometimes a cause can be determined by simple blood tests or scan. But other times more advanced tests must be performed.
Differential diagnosis is the process doctors go through to confirm what the underlying problem is when symptoms point to any number of causes. If the more obvious causes are not confirmed, then the doctor needs to refine the testing. The symptoms of Thymic cancer, where there are symptoms, can point to many underlying issue. Shortness of breath, coughing, pain in the chest can all be caused by so many things. Because Thymic cancers are rare, they might not be the first thing that the doctors suspect. Some of the diseases the doctor has to rule out include:
- Metastatic carcinoma
- Germ cell neoplasms
- Mediastinal large B cell lymphoma
Metastatic Carcinoma must be ruled out before the diagnosis of primary thymic carcinoma is made. This is sometimes called diagnosis by exclusion.
The more experience your doctor has with Thymic cancer, the more likely that doctor will identify the problem quicker.