
The gold standard for Thymic cancer treatment is surgery. Removing all signs of cancer from your body is the best factor for a good prognosis. Often, however, complete resection may require the resection of surrounding involved structures including pericardium, pleura, lung, and even major vascular structures.
 Surgery should be performed by a thoracic surgeon with experience in thymomas and Thymic carcinomas. Unresectable tumors and resectable tumors stage II and above, should be discussed and evaluated by a multidisciplinary team.
Surgery should be performed by a thoracic surgeon with experience in thymomas and Thymic carcinomas. Unresectable tumors and resectable tumors stage II and above, should be discussed and evaluated by a multidisciplinary team.
Thymoma surgery starts with removal of the thymus, called a thymectomy. Unless the tumor is incapsulated, the surgeon will also remove, or attempt to remove, whatever invasion remains. That is the ultimate goal of surgery: complete excision of the cancer with total thymectomy and complete exploration to rule out the presence of noncontiguous disease that may be resectable.
There are several types of thymoma surgery. Your surgeon will decide, with your input, the type of surgery to perform. Some procedures involve more extensive surgery and longer recovery times.
Thymectomy can also be used to treat myasthenia gravis, a neuromuscular disorder that occasionally occurs along with thymomas.
Types of Thymoma Surgery
 Median sternotomy– After creating an incision in front of the breastbone (sternum), the surgeon divides the sternum (sternotomy) to access and remove the thymus, along with any fat on the surface of the heart sac (pericardium) that may harbor cancerous cells. This is the procedure that is commonly needed to completely remove large thymomas, which is usually the case when they are found.
Median sternotomy– After creating an incision in front of the breastbone (sternum), the surgeon divides the sternum (sternotomy) to access and remove the thymus, along with any fat on the surface of the heart sac (pericardium) that may harbor cancerous cells. This is the procedure that is commonly needed to completely remove large thymomas, which is usually the case when they are found.
Transcervical thymectomy – By making an incision across the lower neck, the surgeon is able to access and remove the thymus without dividing the sternum. This approach may be feasible when the thymoma is small, but may not remove all the pericardial far that may harbor separate nests of thymoma cells.
 Minimally invasive techniques, such as Robotic-assisted thymectomy and Video-assisted thoracoscopic surgery(VATS). — The surgeon removes the thymoma through a few small incisions. This approach is particularly useful for small thymomas. During a VATS procedure, a tiny camera (thoracoscope) and surgical instruments are inserted into your chest through one or more small incisions in your chest wall. With VATS, surgeons insert rigid-handled instruments through the incisions, and view the surgery on a flat-screen monitor. In comparison, robotic surgery uses extremely flexible instruments, which can mimic the movement of the human
Minimally invasive techniques, such as Robotic-assisted thymectomy and Video-assisted thoracoscopic surgery(VATS). — The surgeon removes the thymoma through a few small incisions. This approach is particularly useful for small thymomas. During a VATS procedure, a tiny camera (thoracoscope) and surgical instruments are inserted into your chest through one or more small incisions in your chest wall. With VATS, surgeons insert rigid-handled instruments through the incisions, and view the surgery on a flat-screen monitor. In comparison, robotic surgery uses extremely flexible instruments, which can mimic the movement of the human
With large tumors, and invasive ones, complete removal may not be possible with minimally invasive techniques because of the proximity of the tumor to the heart or lungs. Patients need to weigh the benefit of a quicker recovery with potentially not being able to remove everything.
According to the NCCN guidelines:
“Minimally invasive procedures are not routinely recommended due to the lack of long-term data. However, minimally invasive procedures may be considered for clinical stage I–II if all oncologic goals can be met as in standard procedures, and if performed in specialized centers by surgeons with experience in these techniques.”
The Phrenic Nerve
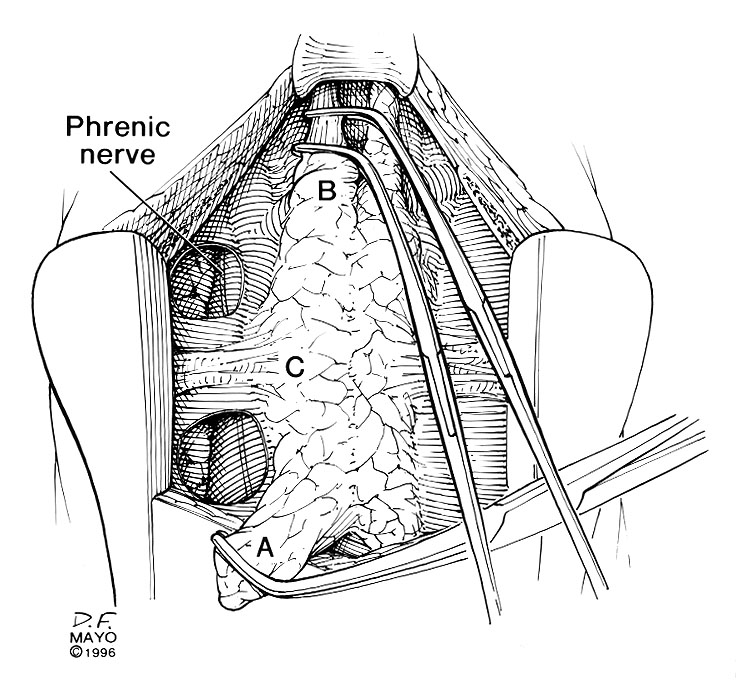
The phrenic nerve is a mixed motor/sensory nerve which originates from the C3-C5 spinal nerves in the neck. From there, the nerve travels downward into the chest to pass between the heart and lungs towards the diaphragm.
The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. Because of its location, the nerve is vulnerable to damage during surgery and this can also cause diaphragmatic weakness, diaphragmatic paralysis or dysfunction. If that nerve is damaged during surgery, there are some actions that can be tried to restore diaphragmatic function.